The Goals of Care Coalition of New Jersey (GOCCNJ) plays a unique and vital role in improving care for older individuals and those living with serious or advanced illness, especially the underserved and most vulnerable. Serving as a catalyst for changes in policy and practice in NJ, we build relationships with and convene key stakeholders and policy makers, advocate to improve access to advance care planning, palliative and hospice care services at the state level, and serve as a resource for those who want accurate, objective information about quality palliative and end-of-life care in NJ.
As a member of the Coalition to Transform Advanced Care (C-TAC), we join other states and actively work towards transforming health care in order to achieve our shared vision that “All Americans with serious illness, especially the sickest and most vulnerable, receive comprehensive, high-quality, person-centered care that is consistent with their goals and values and honors their dignity.” Together with C-TAC, GOCCNJ advocates for federal policies that improve the lives of people with serious illness and those who matter most to them and have committed to advancing health equity and tackling long-standing disparities in serious illness care.
Learn more about GOCCNJ’s current policy priorities that will increase access to palliative and end-of-life care for all people in NJ with serious illness, regardless of race, gender, gender identity, sexual orientation, age, religion, ethnicity, socioeconomic status or where the care is delivered.
Contact us to join our advocacy efforts and improve care for people in NJ with serious illness.
Policy Priorities
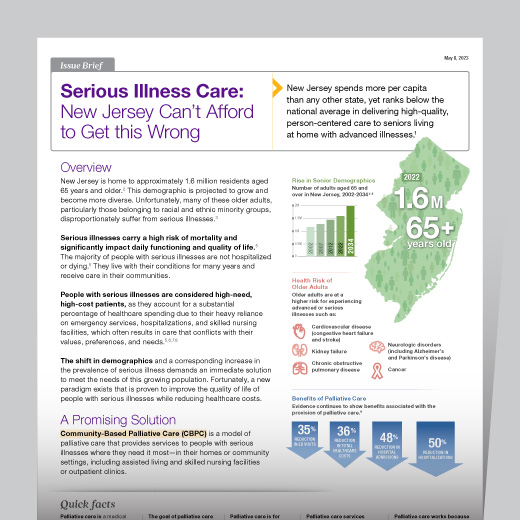
In collaboration with our members and partners, GOCCNJ works to ensure that all individuals living in NJ with serious illnesses, especially those who are underserved and under-resourced, have access to high-quality palliative and end-of-life care. We are committed to addressing barriers to high-quality serious illness care and promoting equity to ensure that all patients in NJ with complex medical needs or serious illness get the care they need and no less, and the care they want and no more.
I. Medicaid Coverage of Community-Based Palliative Care (CBPC)
- Medicaid waivers, state plan amendments, legislation, and other avenues that fund the provision of medically related and non-medical social services that have an impact on health outcomes for people with serious illness as well as legislation that will mandate these services as an essential health benefit for NJ Medicaid beneficiaries living with serious illnessDefinitions and standards that ensure an equitable approach to care
- Public awareness strategies that ensure people living with serious illness and their caregivers understand what CBPC is and how to access it
II. Workforce
- To strengthen and expand the workforce to better care for people with serious illnesses, GOCCNJ supports:
- Expanded workforce training to ensure the workforce’s capacity to deliver services through career development.
- Policies that will enhance professional education and engagement, increase the size of the workforce, and improve the quality and breadth of clinical training.
- Training on serious illness issues in certain medical and health education schools, and development of new curricula on advance care planning and end-of-life care for continuing education.
NJ State Reports
Justice in Aging – Building an Equitable Medicaid HCBS Infrastructure in New Jersey for Older Adults
NJ Department of Human Services Division of Aging Services – State Strategic Plan On Aging
DOH – NJ Governor’s Advisory Council on End-of-Life Care Report and Recommendations
NJHCQI – End-of-Life Strategic Plan for New Jersey
MSNJ – New Jersey Healthcare Executive Leadership Academy 2018
New Jersey Legislature
For more information on the legislature, the members, the legislative process, bills and publications please click the link www.njleg.state.nj.us.
Bill search subject or keyword terms include: serious illness, palliative care, hospice care, healthcare proxy, advance care planning, advance directive, surrogate, end-of-life, long-term care, nursing home.